
Patient Education
Learn more about
your heart
- How the Heart Works
- Inherited Heart Conditions
- Knowing Heart Rhythm
- Signs Of Heart Attack
- Understanding Strokes
- Coronary Hearty Disease
- Congenital Heart Disease
- What is Angina?
- Living with Heart Condition
- Nutrition for Heart Failure
- Nutrition Guide for Diabetes
- Department of Physiotherapy
How The Heart Works?

Your heart is a pump that keeps blood moving around your body. It works 24 hours a day to keep you alive. Each day, your heart beats about 100,000 times.
The heart and its circulation – understanding cardio circulation
Every part of your body needs a fresh supply of blood in order to work normally. It’s your heart’s job to make sure that this is pumped out regularly.
The movement of blood around the body, pumped by the heart, is called circulation. Your heart, blood and blood vessels together make up your cardiovascular system (or heart and circulatory system). Your body contains about five litres (eight pints) of blood, which your heart is continuously circulating.
How blood travels around the heart
The two sides of your heart are separate, but they work together.
The right side of the heart receives dark, de-oxygenated blood which has circulated around your body.
It pumps this to your lungs, where it picks up a fresh supply of oxygen and becomes bright red again. The blood then returns to the left side of the heart, ready to be pumped back out to the rest of your body.
There are four values in your heart. They act like gates that open and close, making sure that your blood travels in one direction through your heart – a bit like one-way traffic system. They are called the tricuspid valve and the pulmonary valve on the right side of the heart, and the mitral valve and the aortic valve on the left.
Like every other living tissue, the heart itself needs a continuous supply of fresh blood. This comes from the coronary arteries which branch off from the main artery (the aorta) as it leaves the heart. The coronary arteries spread across the outside of the myocardium, supplying it with oxygen and essential nutrients.
How blood travels around the body
As your heart muscle contracts, it pushes blood through your heart. With each contraction, or heartbeat:
Your heart pumps oxygenated blood received from the lungs, through the aorta (the main artery leaving the heart) which branches into smaller arteries.
The blood travels through your arteries, which further divides off into even smaller branches of blood vessels called capillaries. Travelling through this network of capillaries, blood reaches every part of your body.
Oxygen is extracted from the blood by tissues and organ in the body after which the de-oxygenated blood then travels back to the heart through your veins. Branches of veins join to form larger veins, which drains blood back to the right side of your heart which will then circulates to the lungs to be oxygenated.
So what can go wrong?
Cardiovascular disease are diseases affecting your heart and circulatory system.
This can occur when your arteries become narrowed by a gradual build-up of fibro-fatty and cholesterol-laden material (called atheroma) within their walls.
The narrowing reduces delivery of oxygen and nutrient rich blood to various parts of your body which can lead to angina, heart attack or stroke, depending on the site of the narrowing.
Inherited Heart Conditions
Inherited conditions can be passed on through families. They can affect many parts of the body or cause many different conditions. They are sometimes called genetic heart conditions.
Inherited heart conditions can affect people of any age and can be life threatening. For many families, the first sign there’s a problem is when someone dies suddenly with no obvious cause or explanation.These conditions are different from most congenital heart conditions, although some congenital conditions can also be inherited.
Our Genes
Our genes make each of us unique. They affect how we look and how our bodies work. We inherit them from our parents. Inherited heart conditions are caused by a fault (or mutation) in one of more of our genes. If one of your parents has a faulty gene, there’s a 50:50 chance you could inherit it. If you do, then there’s also a 50:50 chance you could pass it on to each of your children.
It’s possible to have a faulty gene that can lead to a heart condition, yet never develop any signs of symptoms of the condition itself. You can still pass the gene on and there’s no way of knowing how it may affect your child, even if they do inherit the same faulty gene. Some people with an inherited heart condition do not develop symptoms, yet their child could inherit the same faulty gene and develop symptoms.
What inherited heart conditions are there?
The most common inherited heart conditions are:
- Inherited heart rhythm disturbances, for example:
- Long QT syndrome (LQTS)
- Brugada syndrome
- Catecholaminergic polymorphic ventricular tachycardia (CPVT)
- Progressive cardiac conduction defect (PCCD)
- Cardiomyopathies, for example:
- Hypertrophic cardiomyopathy
- Dilated cardiomyopathy
- Arrhythmogenic right ventricular cardiomyopathy
- Very high cholesterol levels
- Familial hypercholesterolaemia
[/unordered_list]
Who can I speak to about inherited heart conditions?
You should schedule a discussion with any genetic information counsellors who will be able to provide more information and support.They are trained and qualified to advise information about your inherited condition and how it may affect your family.They can help you get an assessment at a specialist clinic that deals with inherited heart conditions.
Abnormal Heart Rhythm

An abnormal heart rhythm – sometimes called an arrhythmia – means your heart is beating too fast, too slow, or with an irregular pattern.Your heart has an electrical system that tells it when to beat and push blood around the body. If there is a problem with this system you may experience an abnormal heart rhythm.
What are the types of abnormal heart rhythm?
There are many different types of abnormal heart rhythm. What type you have depends on where in your heart the rhythm (electrical impulse) starts, and whether it causes your heart to beat too fast, or too slow. The most common abnormal rhythm is atrial fibrillation.
Fast heart rhythms such as supraventricular tachycardia (SVT), inappropriate sinus tachycardia, atrial flutter, atrial fibrillation (AF), ventricular tachycardia (VT) and ventricular fibrillation (VF) are known as tachycardias.
Slow heart rhythms such as AV heart block, bundle branch block and tachybrady syndrome are called bradycardias.
To find out more about these conditions and their treatment, consult specialist medical professionals.
What causes arrhythmia?
There are lots of reasons why you may have a different heart rhythm. Common reasons are:
- The electrical impulses are coming from another part of the heart and not the sinus node.
- The electrical impulses are coming from the sinus node, but going to the lower chambers of the heart by an unusual path.
[/unordered_list]
How does the heart’s electrical system work?
The sinus node is a special group of cells in your heart, also known as your heart’s natural pacemaker.The sinus node sends an electrical signal to the chambers of your heart, which tells them when to contract and push blood through your heart.
If your heart is working properly, the electrical signal will travel from the sinus node to the top chambers of your heart (atria) and then on to the lower chambers (ventricles).
The normal electrical pattern of your heart is known as sinus rhythm. A normal sinus rhythm will generally cause your heart to beat between 60 to 100 beats per minute (bpm) when you’re resting.
My heart rate sometimes feels different. Is this a problem?
It’s normal for your heart to beat at different rates during the day. It will be slower when you’re at rest but may be faster when you are physically active such as when you are gardening, walking briskly, or running. Your heart rate might also be faster if you are anxious or excited.You may experience a sensation of feeling your heart beating whether it is beating normally, quickly, slowly or irregularly. Some people describe them as feeling that your heart is pounding or fluttering. These sensations are called palpitations. For most people, although palpitations can feel unpleasant, they’re usually harmless and do not mean anything is wrong with your heart.
You might also feel that your heart has missed or ‘skipped’ a beat or there has been an extra beat. An extra beat is called an ectopic beat. Ectopic beats are very common and are usually harmless and do not need any treatment.
If you are concerned about palpitations or ectopic beats, you should speak to your doctor who will be able to do an ECG to assess your heart rate and the rhythm.
What are the tests and treatments for abnormal heart rhythms?
Depending on your symptoms, your doctor might recommend that you undergo an ECG – echocardiogram or electrophysiological (EP) study to help diagnose an abnormal heart rhythm.
Depending on the type of abnormal heart rhythm, your doctor may recommend using medication to stop, prevent or control it.
Alternatively, they might suggest a procedure such as cardioversion or catheter ablation, or surgery to insert an implantable cardioverter defibrillator (ICD) or pacemaker.
Abnormal Heart Rhythm

Did you know that a heart attack is seriously life threatening? A heart attack happens when your heart is starved of oxygen-rich blood – this causes damage to your heart muscle.
What are the signs of a heart attack?
- Chest pain – tightness, heaviness, pain or a burning feeling in your chest region
- Pain in arms, neck, jaws, back ort stomach – for some people, the pain or tightness is severe, while for others, they just feel uncomfortable
- Sweating
- Feeling light-headed
- Short of breath
- Nauseous or vomiting
[/unordered_list]
What causes a heart attack?
Most heart attacks are caused by coronary heart disease. Coronary heart disease (CHD) is when your coronary arteries (the arteries that supply your heart muscle with oxygen-rich blood) become narrowed by a gradual build-up of fatty material within their walls.
If a piece of this fatty material (atheroma) breaks off it may cause a blood clot (blockage) to form. If it blocks your coronary artery and cuts off the supply of oxygen-rich blood to your heart muscle, this is a heart attack.
You might also hear a heart attack called acute coronary syndrome, myocardial infarction (MI) or coronary thrombosis.
Other rarer causes of a heart attack include spontaneous coronary artery dissection(SCAD) where one or more of the coronary arteries tear.
What happens to the heart after a heart attack?
A heart attack always causes some permanent damage to your heart muscle, but the sooner treatment is given, the more muscle it is possible to save.
If a heart attack damages a significant amount of your heart muscle, this can affect the pumping action of your heart. The term used to describe this is heart failure.
Also, some people continue to get angina after they have had treatment for their heart attack, because there is still narrowing of one or more of their coronary arteries.
How do you diagnose a heart attack? (On the way to a hospital and in an ambulance)
- Examination and monitoring of the heart rate and blood pressure
- Perform an electrocardiogram (ECG) in the ambulance
- Assessment of symptoms and medical history,
- Provision of pain relief if needed and oxygen if the oxygen level is too low
- Provision of aspirin if not given already
- Transfer to the most suitable hospital.
[/unordered_list]
What happens at the hospital?
- When you arrive at hospital you will receive treatment for your blocked artery.
- Either you will have a Primary Percutaneous Coronary Intervention (PPCI) which is an emergency coronary angioplasty. It involves reopening your blocked coronary artery, restoring the blood supply to the part of your heart that is starved of blood, which helps to save as much of your heart muscle as possible.
- Or you will have Thrombolysis, also called a ‘clot buster’. This involves injecting a medicine into a vein to dissolve the blood clot and restore the blood supply to your heart. Sometimes this may be given to you in the ambulance.
- In some types of heart attack people do not receive either of these two treatments because they will not benefit from them.
[/unordered_list]
What about recovery?
A heart attack can be a frightening experience and it can take time to come to terms with what has happened. It’s natural to be worried about your recovery and future.
Many people make a full recovery and within a few months are able to return to their normal activities.
However some people may find that they are not able to do as much as they previously did. Attending a cardiac rehabilitation course will increase your chances of getting back to normal as quickly as possible.
Stroke And Your Heart
Your brain needs a constant supply of blood to work properly.A stroke happens when the blood supply to part of your brain is cut off, causing your brain cells to become damaged or die.
The two most common types of stroke are ischaemic and haemorrhagic stroke:
- ischaemic strokes happen when the artery that supplies blood to your brain is blocked, for example by a blood clot.
- haemorrhagic strokes happen when a blood vessel bursts and bleeds into your brain, damaging brain tissue and starving some of your brain cells of blood and oxygen.
[/unordered_list]
Without a constant blood supply, your brain cells will be damaged or die, which can affect the way your body and mind work.
What are the symptoms of stroke?
Act F.A.S.T to recognise the symptoms.
Facial weakness – can they smile? Has their mouth or eye drooped? Arm weakness – can they raise both arms? Speech problems – can they speak clearly and can they understand what you are saying? Time – Respond to the condition – if you think someone is having a stroke, call for an ambulance.
What is a mini stroke or TIA?
A transient ischaemic attack (also called a TIA or mini-stroke) happens when there is a temporary blockage in the blood supply to the brain. A TIA doesn’t cause permanent damage to your brain and the symptoms usually pass within 24 hours.
It’s often hard to tell the difference between a stroke or TIA, so if you think someone is having a TIA you should still call the ambulance. A TIA can be an important warning that there is a problem with the blood supply to your brain.
Also, some people continue to get angina after they have had treatment for their heart attack, because there is still narrowing of one or more of their coronary arteries.
What is the relationship between a stroke and the heart?
- Coronary heart disease (angina and heart attack) and stroke can be caused by the same problem – atherosclerosis. This is when your arteries become narrowed by a gradual build-up of fatty material (called atheroma) within their walls.
- If a piece of atheroma breaks away from one of your arteries it will lead to a blood clot forming.If the blood clot blocks an artery to your heart and cuts off the blood supply to your heart muscle, this is a heart attack.
- If the blood clot blocks an artery to your brain and cuts of the blood supply, this is anischaemic stroke.
- If you have atrial fibrillation (AF) your risk of stroke is increased by around four to five times. This is because AF increases the risk of a blood clot forming inside the chambers of your heart. This clot can travel through your bloodstream and block the blood supply to your brain – causing a stroke.
[/unordered_list]
What are the risk factors for stroke?
A risk factor is something that that increases your likelihood of getting a disease. The more risk factors you have, the more likely you are to have a stroke.
Take a look at our cardiovascular disease page to find out about the risk factors for stroke and other cardiovascular diseases such as coronary heart disease.
Coronary Hearty Disease (CHD)
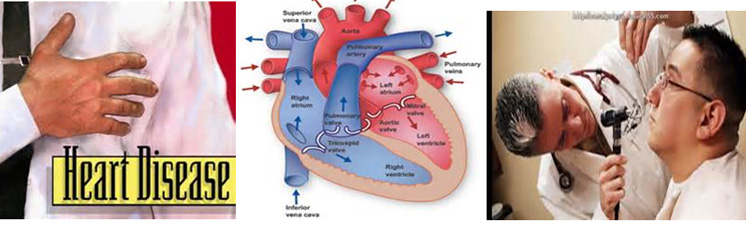
Coronary heart disease (CHD) is when your coronary arteries (the arteries that supply your heart muscle with oxygen-rich blood) become narrowed by a gradual build-up of fatty material within their walls.
This condition is called atherosclerosis and the fatty material is called atheroma.
In time, your arteries may become so narrow that they cannot deliver enough oxygen-rich blood to your heart. The pain and discomfort you may feel as a result is called angina.
If a piece of atheroma breaks off it may cause a blood clot (blockage) to form. If it blocks your coronary artery and cuts off the supply of oxygen-rich blood to your heart muscle, your heart may become permanently damaged. This is known as a heart attack.
Risk factors for coronary heart disease
A risk factor is something that that increases your likelihood of getting a disease. There are several factors that can increase the risk of developing CHD. The main ones are:
- Smoking
- High blood pressure
- High blood cholesterol
- Diabetes
- Being physically inactive
- Being overweight or obese
- Family history of heart disease
- Ethnic background
- Sex – men are more likely to develop CHD at an earlier age than women.
- Age – the older you are, the more likely you are to develop CHD.
[/unordered_list]
The more risk factors you have, the more likely you are to develop CHD. Even though you can’t change all your risk factors, there is plenty you can do to reduce your risk and help to protect your heart.
CHD diagnosis and risk assessment
You will need a health and heart check to assess your risk of coronary heart disease if you are between 40 and 74 years old.
There are many types of heart check up. At IJN, the healthcare professional will check your blood pressure and cholesterol levels and talk to you about your lifestyle. Based on the results, they will give you practical advice about keeping your heart healthy.
If you have a heart problem already, is there any treatment?
Your doctor will discuss treatment options with you, depending on the type of heart problem that you have. These may vary from taking medication, to having surgery or a medical procedure.Even if you already have a heart condition it’s still really important protect your heart byliving a healthy lifestyle.
Congenital Heart Disease
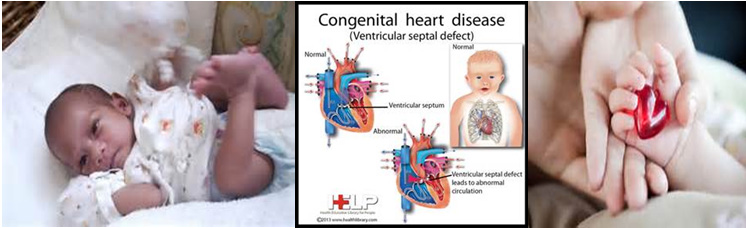
Congenital heart disease means a heart condition or defect that develops in the womb, before a baby is born.There are many different types of congenital heart disease. For example, a baby’s heart valves may not be properly formed or there may be holes between the chambers of their heart.
For many babies diagnosed with congenital heart disease, their condition is a minor problem which either doesn’t need any treatment or can be successfully corrected with surgery. Other conditions are more serious and sadly, some children do not survive. However, thanks to advances in early diagnosis and treatment, most children will grow up to become adults and lead full and active lives.
What causes congenital heart disease?
In most cases, something has gone wrong in the early development of the foetus. Some heart conditions are due to faulty genes or chromosomes. But often we don’t understand why the baby’s heart hasn’t developed normally.
If there’s a family history of congenital heart disease, the mother has diabetes during pregnancy, or the mother has taken certain medications while pregnant (anticoagulants or antiepileptics) a baby may be at slightly higher risk of congenital heart disease.
How is congenital heart disease detected?
Some congenital heart problems are now picked up when the mother has an ultrasound scan during pregnancy (usually at the 20-week scan), but sometimes they are not found until after the baby has been born. Some conditions may not be discovered until the child is older or even an adult.
In babies and toddlers, congenital heart disease can have a range of symptoms because every child and condition is different. More common symptoms include extreme tiredness, poor feeding, excessive sweating, rapid heartbeat, breathing problems, chest pain and a blue tinge to the skin. If you notice any of these symptoms in your child, you should seek medical attention.
The more risk factors you have, the more likely you are to develop CHD. Even though you can’t change all your risk factors, there is plenty you can do to reduce your risk and help to protect your heart.
If a congenital heart condition is suspected after your 20-week pregnancy scan
You may be asked to attend another scan with a specialist or referred to a fetal medicine unit, obstetrician or a specialist in cardiac or child medicine.
If a congenital heart condition is confirmed, you should be given a detailed description of the problem, information about any surgery that might be needed, and the overall long-term outlook.
If appropriate, specialist monitoring and care will be provided before, during and after the birth so that your baby can receive tests and treatment as soon as possible. Some heart conditions can now also be treated in-utero (in the womb) before the birth.
If a congenital heart condition is suspected in a baby or child
Your child may undergo a physical examination and heart tests such as an ECG.If the diagnosis is confirmed, they will be seen by a paediatric cardiologist, who will manage their care. You should be given a detailed description of the problem, information about any surgery that might be needed, and the overall long-term outlook for your child.
What treatment is available?
Treatment depends on the type and severity of the condition. Some children won’t require any treatment while others may need medication or heart surgery. There are also other new techniques and procedures that, in some cases, can be done instead of surgery.
Regardless, you need to consult specialized professional medical help. You will need a detailed and thorough understanding of your child’s heart and the different heart conditions. The medical professionals will discuss symptoms and treatments, and where to go for more support.
Angina
Angina is a pain or discomfort felt in your chest, which is usually caused by coronary heart disease.Some people feel the pain in their arm, neck, stomach or jaw.
What causes angina?
Angina is usually caused by coronary heart disease. When the arteries that supply your heart muscle with blood and oxygen become narrowed, the blood supply to your heart muscle is restricted. This can cause the symptoms of angina.
Angina symptoms are often brought on by physical activity, an emotional upset, cold weather or after a meal. The episodes usually subside after a few minutes.
Other causes of angina
There are two other causes of angina. Variant angina (also known as Coronary artery spasm or Prinzmetal’s angina) happens when a coronary artery supplying blood and oxygen to your heart goes into spasm.
Cardiac syndrome X (also known as microvascular angina) usually occurs when you’re exerting yourself, for example when you’re physically active, or have had an emotional upset. With cardiac syndrome X, your coronary arteries will appear normal when they’re investigated, and there will be no evidence of the atheroma (fatty build-up in your arteries) that usually causes angina.
The more risk factors you have, the more likely you are to develop CHD. Even though you can’t change all your risk factors, there is plenty you can do to reduce your risk and help to protect your heart.
Angina symptoms
Angina often feels like a heaviness or tightness in your chest, and this may spread to your arms, neck, jaw, back or stomach as well. Some people describe a feeling of severe tightness, while others say it’s more of a dull ache. Some people experience shortness of breath too.
If you think your angina has got worse, feels different than it has before, has become more frequent, or has changed in any other way, you should consult a doctor immediately.
What should I do if I get chest pains?
If you have not been diagnosed with angina and experience chest pain, call for an ambulance immediately.
If you have already been diagnosed with angina, you may experience angina pain or discomfort that you can manage by taking your glyceryl trinitrate (GTN) spray or tablets, and resting.
However, it could be a heart attack so if you feel:
- a crushing pain, heaviness or tightness in your chest.
- a pain in your arm, throat, neck, jaw, back or stomach.
- become sweaty, feel light-headed, sick or become short of breath.
[/unordered_list]
You can take these steps:
- Stop what you are doing and sit down and rest.
- Take your GTN spray and tablets, according to your doctor or nurse’s instructions. The pain should ease within a few minutes – if it doesn’t, take a second dose.
- If the pain does not ease within a few minutes after your second dose, call 999 immediately.
- If you’re not allergic to aspirin, chew one adult tablet (300mg). If you don’t have any aspirin or you are not sure if you’re allergic to aspirin, you should rest until the ambulance arrives.
- Even if your symptoms don’t match the above but you suspect you’re having a heart attack, call for an ambulance immediately.
[/unordered_list]
Living With A Heart Condition

When you’ve been diagnosed with a heart condition it’s natural to need time to come to terms with what has happened to you and how your everyday life may be affected.
Cardiac Rehabilitation
Cardiac rehabilitation is a programme of exercise and information sessions to help you get back on your feet again after a heart attack, heart surgery or procedure. It helps you to:
- understand your condition
- recover from your surgery, procedure or heart attack
- make changes to your lifestyle that will help improve your heart health
- reduce the risk of further heart problems.
[/unordered_list]
Who is cardiac rehab for?
Cardiac rehabilitation is available to anyone who has had:
- a heart attack
- a coronary angioplasty
- heart surgery
- those who have angina or heart failure
- those who have an ICD implanted.
[/unordered_list]
When does one start?
Cardiac rehabilitation starts as soon as you go into hospital for heart surgery or treatment, or after you’ve had a heart attack.
A member of the cardiac rehabilitation team will normally visit you on the ward to provide you with information about your condition, the treatment you’ve had and your recovery. This will help you get back to your usual activities as soon as possible.
You should also be invited to join a cardiac rehabilitation programme starting about four to eight weeks after you leave hospital.
Nutrition for Heart Failure
In heart failure, the body often retains fluid, leading to:
- Increased blood pressure (heart needs to work harder)
- Shortness of breath (due to fluids in the lungs)
- Swelling on ankles, face and hands
- Nausea and bloating
[/unordered_list]
Tips for fluid control
- Use measuring cups to accurately measure your fluid intake.
- Spread your fluid allowance over the day.
- Use a small rather than large cup.
- Remember to include food that contains large amount of fluid. (E.g. Fruits, soup etc.)
- Limit salt and salty foods as these make you thirsty.
- Brush your teeth, gargle with mouthwash or try mint/chewing gum to freshen your mouth.
- Suck slowly on lemon slices or frozen fluids from your allowance
[/unordered_list]
Salt Intake
Too much salt in your diet can make the body hold on to water. It may worsen symptoms such as swelling, bloating and shortness of breath. Therefore, your heart has to work harder to pump around this extra fluid in the body.
Tips to reduce salt intake
- Limit intake of high salt food and go easy on condiments and sauces.
- Choose products labelled “low salt” or “no added salt”.
- Choose fresh foods instead of processed food such as canned, cured, pickled foods.
- Minimize added salt at the table or in cooking.
- Use natural herbs, spices, pepper, lemongrass, garlic, onion, shallots, lemon, tomato, vinegar to add flavour to foods.
- Make stock by boiling chicken, meat bones, and vegetables instead of using stock cubes or powders.
- Choose meehoon or kueyteow over yellow noodles which is higher in salt
[/unordered_list]
Referral to the Dietitian
For more nutrition information and consultation, please contact IJN’s Diet Clinic:
Diet Clinic Block A: 03-26006596
Diet Clinic Block B: 03-26006942
What is Carbohydrate?
Carbohydrate food group is converted into glucose before adsorbed into our bloodstream to be utilize as energy by the body cells for daily activity.
Sources of carbohydrate includes:
- Cereals and grains such as rice, noodles, bread
- Starchy vegetables such as potato, pumpkin, sweetcorn, yam
- Legumes and lentils
- Fruits
- Milk and dairy products
- Sweeteners and sweetened products
[/unordered_list]
Having diabetes does not mean to discourage you from eating carbohydrates but do take control of the portion size of these food. Discuss with a dietitian about your required carbohydrate allowance in a day.
Tips to Control Diabetes
- Manage Your Body Weight
Achieving normal body weight helps to regulate your blood glucose. If you are overweight, consider to work with your dietitian to lose some weight. Studies have shown that 5% reduction of your current body weight can improve your diabetes control. A Body Mass Index (BMI) of 18.8 – 24.9 kg/m2 is considered healthy. You can calculate your BMI with the following formula:
BMI = Weight (kg) / Height (m) x Height (m) - Choose Your Carbohydrate Intake Wisely
There are basically two types of carbohydrates in the diet: sugars and starches.
Examples of sugars include table sugar, honey and the natural sugars found in milk and fruits. Examples of starches are grains and grain products (e.g. rice, noodles, bread, oats, chapatti and biscuits), starchy vegetables (e.g. potato and pumpkin), beans and lentils.- Limit consumption of sugar sweetened food and drinks
Sugar sweetened food and drinks are mostly high in calories and low in nutrient. Avoid excessive intake of sugar sweetened products. Substitute added sugars with artificial sweeteners to avoid spikes in blood sugar levels. - Make half your grains whole
Include fiber-rich starches such as brown rice, whole meal bread as part of a well-balanced diet. They are usually nutrient-dense and will also help with blood glucose control.
- Limit consumption of sugar sweetened food and drinks
- Eat at Regular Mealtimes
Avoid skipping meals and have your meals on time especially if you are on insulin to prevent getting hypoglycemia or possibly overeat at the next meal due to hunger. - Check Your Blood Glucose Levels
Own a glucometer to monitor your blood glucose regularly. - Commit to Regular Exercise
Perform aerobic exercises for 150 minutes in a week or aim for about 30 minutes a day, at least 5 days in a week. If you have not been very active recently, start your routine with 5 to 10 minutes a day then step up each week. Choice of exercise can be in brisk walking, climbing stairs, swimming or cycling.
[/unordered_list]
Referral to the Dietitian
For more nutrition information and consultation, please contact IJN’s Diet Clinic:
Diet Clinic Block A: 03-26006596
Diet Clinic Block B: 03-26006942
Department Of Physiotherapy, Ijn.
Introduction
- The objective of the Physiotherapy Department is directed towardspatient achieving an optimal level of physical and socialindependence and improving quality of life.
- Our team of physiotherapists work together to provide a complete continuum of quality physiotherapeutic care to IJN’s patients – preventive, rehabilitative and maintenance.
[/unordered_list]
Our Services
- Cardiothoracic and Cardiopulmonary care
- Cardiac Rehabilitation Program
- Pain Management services
- Special test / Diagnostic Test
- Cardio fitness Program
- Patient education on physical activities
[/unordered_list]
We are located at:
Ground floor, Block B,
National Heart Institute,
145, JalanTunRazak,
Kuala Lumpur
Tel: 03- 2617 8339
Cardiothoracic and Cardiopulmonary Care
Introduction
Cardiorespiratory endurance refers to the ability of the circulatory and respiratory systems to supply oxygen to skeletal muscles during sustained physical activity. Early mobilization and physical activity improves the respiratory system by increasing the amount of oxygen that is inhaled and distributed to body tissue.
Active/Passive Exercise
Active/passive exercise are done through the whole range of motion of the joint to preserve flexibility and mobility of the joints on which they are performed. These exercises maintain existing joint and soft-tissue mobility, minimize effects of the formation of contractures & improves sensory feedback from the contracting muscles.
AMBULATION
The ability to walk from one place to another independently with or without assistive device is the ultimate goal of the patient. To be able to move (especially walking), prevents cardio-pulmonary and musculoskeletal complications such as reduced cardiovascular endurance, muscular dystrophy, loss of coordination and stability as well as reverse anxiety and disease related stress.
Breathing/Airway Clearance
- Definition:To mobilize and clear excess bronchial secretions from the lungs. Frequently executed with a combination of manual therapy such as postural drainage (percussion & vibration), special breathing techniques and effective coughing and warm humidified steam therapy to enhance airway clearance.
- Incentive Spirometry allows patients to perform sustained maximal inspiration (SMI) without added resistance while presenting a visual feedback of the inspiratory effort. It increases transpulmonary pressure and inspiratory volumes, improves inspiratory muscle performance, and simulate the normal pattern of pulmonary hyperinflation.
[/unordered_list]
Cardiac Rehabilitation Program
Introduction
Cardiac rehabilitation is a continuous process of care which begins in the hospital. This program designed specifically for your needs, includes exercise, lifestyle changes, education, and emotional support from a multidisciplinary team. It can help improve your health and enable you to live a more active and quality life. Cardiac rehab can also help you return to work safely and in a timely manner.
Cardiac Rehabilitation can be divided into 3 phases:
Phase 1
This is the period of time when patients are admitted in hospital for a cardiac event. With supervision from the physiotherapist, patients begin with non-strenuous activities, such as sitting up in bed, breathing exercise, range-of-motion exercises and self-care, such as shaving. The program then progresses to walking and low intensity exercises either in the wards or gymnasium.
Phase 2
This is done in an outpatient setting upon discharge from the hospital. The Cardiac Rehab Phase II program is a structured, medically supervised, outpatient program for patients with heart disease that incorporates regular exercise ( group and circuit training ) along with other services such as nutritional education, stress management, and smoking cessation. In IJN, our Cardiac Rehabilitation Program Phase II may start as early as 2-3 weeks post-surgery or cardiac event.
Phase 3
This phase is a long term maintenance program. At this point, you probably would have developed your own exercise routine at home or at a local gym. The challenge now is to maintain a regular exercise program for the rest of your life.
Pain Management Services
- The use of electrotherapeutic modalities to relieve or reduce pain. These include TENS, Hot pack, Laser therapy, Ultrasound, Cryotherapy.
[/unordered_list]
1) Transcutaneous Electrical Nerve Stimulation (TENS)
Induces pain relief for headaches, acute post-operative pain, arthritis, Phantom limb and low backache.
2) Hot pack
Suitable for soft tissue Injuries, muscles spasm, acute &superficial inflammatory conditions or for those contraindicated for electrical modalities.
Contra-indication:
- Psychological
- Skin insensitivity
- Peripheral nerve injuries e.g. numbness, impaired sensation.
- Vasospastic diseases
- Peripheral vascular disease (decreased circulation)
- Cold insensitivity.
[/unordered_list]
3) Cryotherapy (Ice Pack)
For relieving or reduce pain, reduce spasticity, reduce muscle spasm, reduce swelling, promote repair and provide excitatory stimulus when muscles are inhibited
Contra-indication:
- Psychological treat
- Peripheral nerve injuries with impaired sensation.
- Vasospastic diseases
- Peripheral vascular disease
- Cold sensitivity.
[/unordered_list]
4) Light amplification by stimulated emission of radiation (LASER)
LASER is used as a pain relief modality in conditions such as painful shoulder, hip arthrosis, epicondylitis, carpel tunnel syndrome etc. LASER heals the tissue while providing a powerful and non-addictive form of pain management by blocking pain pathways in the nervous systems and brings immediate pain relief.
Contra-indication:
- Pacemaker
- Pregnancy
- Epileptic seizures
- Thyroid gland
- Active cancer/malignancy
[/unordered_list]
5) Ultra Sound Therapy
Ultrasound is a therapeutic modality used for the treatment of acute & chronic condition affecting ligaments, tendons and muscle tissue. It is also used to achieve muscle relaxation and pain reduction by improving blood perfusion and recovery of injured tissue.
Contra-indication:
- Vascular condition
- Pregnancy
- Acute infections
- Severe ischemic areas
- Radiotherapy
- The nervous system
- Tumors
- Metal implant
[/unordered_list]
SPECIAL TEST/ DIAGNOSTIC SERVICES
Breath CO test
- The test is used to measure the amount of Carbon Monoxide (CO2) in your lungs and blood.
- This is an indirect, non-invasive measure of blood carboxyhemogblobin (%COHb), which is the level of CO in your blood
[/unordered_list]
Lung Function Test
- Lung function tests provides a guide to the state and function of the respiratory system.
- Monitors the progress of the disease or response to treatment.
- To assess- and define the degree or severity of the disease or disability.
[/unordered_list]
Six Minute Walk Test ( 6MWT )
- The test is used as a performance-based measure of functional exercise capacity.
- The test is used as a measure of the response to medical interventions in patients with moderate to severe heart or lung disease.
[/unordered_list]
Introduction
- A diagnostic test is any kind of medical test performed to aid in the diagnosis or detection of disease, injury or any other medical condition
- It may be used to confirm that a person is free from a disease, or to fully diagnose a disease, including sub-classifying it according to the severity and susceptibility to treatment.
- A Special test is important to obtaining an accurate diagnosis, and in turn maximizing treatment outcomes.
[/unordered_list]
Body Composition Analysis / Body Impedance Analysis
- This method measures body composition by sending a low, safe electrical current through the body.
- The current passes freely through the fluids contained in muscle tissue, but encounters difficulty/resistance when it passes through fat tissue. This resistance of the fat tissue to the current is termed ‘bioelectrical impedance’.
- When set against a person’s height, gender and weight, the scales can then compute their body fat percentage, lean muscle mass, total percentage of water and minerals.
[/unordered_list]
Cardio Fitness Program
Introduction
This is progression of the Cardiac Rehabilitation Program in the later stages following a cardiac event. It is also applicable to those with one or more risks factors of cardiovascular disease to improve cardiovascular fitness and take change of self- management strategies of life long behavioral changes.
A series of tests and medical screening will be carried out prior to a prescribed exercise program in a safe environment with top medical facilities.
The client will go through a strict risk stratification which will be reviewed by a doctor to determine suitability for the program.
Suitable for:
- All physically fit individual
- Sedentary people
- Those who want to change lifestyle
- Those who wants to improve cardiovascular fitness
- Those with one or more coronary risk factors for heart disease
[/unordered_list]
Benefits of CFP
- Stimulates production of red blood cells
- Improves resistance to infection
- Develops alertness, awareness & lessens reaction time Between brain and body.
- Decrease hazard of diabetes
- Improve blood circulation in the legs.
- Strengthens heart muscle – reduces high blood pressure and heart rate
- Improves cardiovascular endurance and exercise tolerance.
[/unordered_list]
Contraindication
- Unstable or unresolved angina.
- Fever and acute systemic illness.
- Patient in severe pain.
- Resting blood pressure: SBP> 180mmHg, DBP> 100mmHg
- Significantly unexplained drop in blood pressure.
- Tachycardia > 100bpm.
- New or recurrent symptoms of breathlessness, palpitation, dizziness.
- Significant lethargy.
[/unordered_list]
For more information, please contact:
Tel: +603- 2617 8339
Fax: +603- 2600 6545
Email: cfp@ijn.com.my
Website: www.ijn.com.my
Patient education on Physical Activities Post Cardiac Event
Introduction
Education on physical activities throughout the recovery process is essential to prevent and eliminate adverse lifestyles and behaviors and specific interventions such as smoking cessation, dietary modification and exercise are recommended to prevent recurrences and slow the progression of disabling complication.
Objective:
- Provide health information on the (coronary) disease process and therapeutic interventions aimed at slowing, halting or reversing the progression.
- Allows the patient the freedom to discuss any queries or concerns regarding social and home activities.
- Prepare patients for a return to work and resumption of activities of daily living at home and in the community.
- Equip patients with the knowledge on how to progress with their exercise training program safely and appropriately within the constraints of their medical condition.
[/unordered_list]
Benefit of exercise:
- Regular activity strengthens your heart muscle
- Lowers blood pressure
- Increases high- density lipoproteins or HDLs.
- Lowers low-density lipoproteins or LDLs.
- Enhances blood flow.
- Helps your heart function more efficiently.
- Gives you more energy
- Improves your mood.
- Helps you manage your weight.
- Promotes better sleep.
[/unordered_list]
